Modern and advanced Semen Analysis treatment with guaranteed results
Semen analysis, also known as a sperm count test, analyzes the health and viability of a man’s sperm.
THE LIFE PLUS HOSPITAL Care is COVID 19 Safe
1. Our Hospital premises are COVID safe
2. Regular sanitization of clinic & hospital premises
3. Immediate medical assistance through Online Consultation
Modern and advanced Semen Analysis treatment with guaranteed results
Semen analysis, also known as a sperm count test, analyzes the health and viability of a man’s sperm.
THE LIFE PLUS HOSPITAL Care is COVID 19 Safe
- Our Hospital premises are COVID safe
- Regular sanitization of clinic & hospital premises
- Immediate medical assistance through Online Consultation

Semen Analysis
Semen analysis, also known as a sperm count test, analyzes the health and viability of a man’s sperm. Semen is the fluid containing sperm (plus other sugar and protein substances) that’s released during ejaculation. A semen analysis measures three major factors of sperm health:
- the number of sperm
- the shape of the sperm
- the movement of the sperm, also known as “sperm motility”
Doctors will often conduct two or three separate sperm analyses to get a good idea of sperm’s health. According to the American Association for Clinical Chemistry (AACC), the tests should be conducted at least seven days apart and over the course of two to three months. Sperm counts can vary on a daily basis. Taking an average of the sperm samples can give the most conclusive result.
Let's Schedule Your Appointment
Treatment
What is checked in a semen analysis?
A semen analysis will check for a number of things, including:
- Semen volume (the amount that you ejaculate)
- Sperm concentration (also known as sperm count, meaning the number of sperm per milliliter of semen)
- Total sperm number
- Sperm motility (the number of moving sperm compared to non-moving sperm)
- Sperm vitality (the number of ‘alive’ sperm)
- The number of ideally shaped sperm (normal sperm) compared to oddly shaped sperm (abnormal sperm)
- White blood cells (which can be a sign of infection)
- Semen pH (to see if you’re semen is acidic or alkaline; it should be slightly alkaline)
- Sperm antibodies (a protein that fights sperm).
Our Doctors
Why The Life Plus Hospital?
 The Life Plus Hospital is COVID-19 safe
The Life Plus Hospital is COVID-19 safe
Your safety is taken care of by thermal screening, social distancing, sanitized clinics, and hospital rooms, sterilized surgical equipment, and mandatory PPE kits during surgery.
 Medical Expertise With Technology
Medical Expertise With Technology
Our Doctors spend a lot of time with you to diagnose your condition. You are assisted in all pre-assisted Hospitalisation process. We offer advanced laser and laparoscopic surgical treatment. Our procedures are USFDA approved.
 Assisted Surgery Experience
Assisted Surgery Experience
A dedicated Medical Coordinator assists you throughout the surgery journey from insurance paperwork, to free commute from home to hospital & back and admission-discharge process at the hospital.
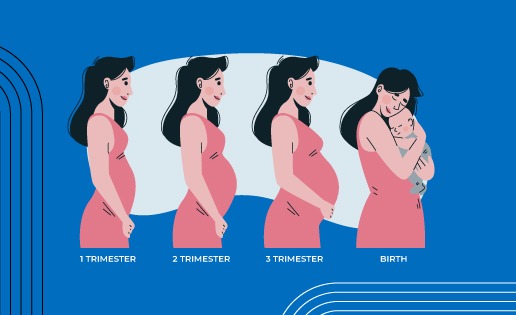
 Post Natal Care
Post Natal Care
We offer free follow-up consultations and instructions including dietary tips as well as exercises to every patient to ensure they have a smooth recovery to their daily routines.
The Life Plus Hospital in Numbers
IVF / ICSI
Surrogacy
IUI
Healthy IVF Babies
What is a semen analysis?
A semen analysis, also called a sperm count, measures the quantity and quality of a man’s semen and sperm. Semen is the thick, white fluid released from the penis during a man’s sexual climax (orgasm). This release is called ejaculation. Semen contains sperm, the cells in a man that carries genetic material. When a sperm cell unites with an egg from a woman, it forms an embryo (the first stage of an unborn baby’s development).
A low sperm count or abnormal sperm shape or movement can make it difficult for a man to make a woman pregnant. The inability to conceive a baby is called infertility. Infertility can affect men and women. For about one-third of couples unable to have children, male infertility is the reason. A semen analysis can help figure out the cause of male infertility.
Other names: sperm count, sperm analysis, semen testing, male fertility test
What is it used for?
A semen analysis is used to find out if a problem with semen or sperm may be causing a man’s infertility. The test may also be used to see if a vasectomy has been successful. A vasectomy is a surgical procedure that is used to prevent pregnancy by blocking the release of sperm during sex.
Why do I need a semen analysis?
You may need a semen analysis if you and your partner have been trying to have a baby for at least 12 months without success.
If you’ve recently had a vasectomy, you may need this test to make sure the procedure has worked.
What happens during a semen analysis?
You will need to provide a semen sample. The most common way to provide your sample is to go to a private area in your health care provider’s office and masturbate into a sterile container. You should not use any lubricants. If masturbation is against your religious or other beliefs, you may be able to collect your sample during intercourse using a special type of condom. Talk to your health care provider if you have questions or concerns about providing your sample.
You will need to provide two or more additional samples within a week or two. That’s because sperm count and semen quality can vary from day today.
Will I need to do anything to prepare for the test?
You will need to avoid sexual activity, including masturbation, for 2–5 days before the sample is collected. This will help make sure your sperm count is at its highest level.
Are there any risks to the test?
There is no known risk to semen analysis.
What do the results mean?
The results of semen analysis include measurements of quantity and quality of semen and sperm. These include:
- Volume: the amount of semen
- Sperm count: the number of sperm per milliliter
- Sperm movement, also known as motility
- Sperm shape, also known as morphology
- White blood cells, which may be a sign of an infection
If any of these results are not normal, it may mean there is a problem with your fertility. But other factors, including the use of alcohol, tobacco, and some herbal medicines, can affect your results. If you have questions about your results or other concerns about your fertility, talk to your health care provider.
If your semen analysis was done to check the success of your vasectomy, your provider will look for the presence of any sperm. If no sperm is found, you and your partner should be able to stop using other forms of birth control. If sperm is found, you may need repeat testing until your sample is clear of sperm. In the meantime, you and your partner will have to take precautions in order to prevent pregnancy.
What is checked in a semen analysis?
A semen analysis will check for a number of things, including:
- Semen volume (the amount that you ejaculate)
- Sperm concentration (also known as sperm count, meaning the number of sperm per milliliter of semen)
- Total sperm number
- Sperm motility (the number of moving sperm compared to non-moving sperm)
- Sperm vitality (the number of ‘alive’ sperm)
- The number of ideally shaped sperm (normal sperm) compared to oddly shaped sperm (abnormal sperm)
- White blood cells (which can be a sign of infection)
- Semen pH (to see if you’re semen is acidic or alkaline; it should be slightly alkaline)
- Sperm antibodies (a protein that fights sperm).
How is semen collected for testing?
Semen testing should be done with a fresh semen sample ejaculated within one hour of examination. A semen sample is best collected in a specimen jar and produced by masturbation. You usually do this in a private room at the testing laboratory. When you collect semen at home, you have to keep the sample warm and take it to the laboratory very quickly – within one hour if possible. If this method of collecting semen is too difficult, you can talk to your doctor about alternatives.
You need to make sure that you don’t lose any of the semen sample. As sperm are mostly in the first part of the ejaculate, losing the first part can falsely lower the sperm concentration. It’s important that you don’t ejaculate for at least two days before the sample is collected, but it’s equally important that it’s not been longer than seven days since you last ejaculated.
World Health Organization Guidelines for Normal Semen Analysis
Your doctor will explain your results to you. Different labs and physicians sometimes use different normal value ranges. Keep in mind that what your doctor considers to be normal or abnormal might differ from the values listed here.
| Parameter | Lower Reference Limits |
| Semen volume (ml) | 1.5 (1.4 to 1.7) |
| Total sperm count (10^6) | 39 (33 to 46) |
| Sperm concentration (10^6 / ml) | 15 (12 to 16) |
| Total motility (percent) | 40 (38 to 42) |
| Progressive motility (percent) | 32 (31 to 34) |
| Vitality (percent) | 58 (55 to 63) |
| Sperm morphology (percent) | 4 (3 to 4) |
WHO lower reference values for semen characteristics
These semen parameters are only guidelines to consider when investigating what could be causing your infertility. Having better or worse numbers than what is listed here does not necessarily mean that you will or won’t be able to father a child.
What do the results of a semen analysis mean?
A semen analysis doesn’t guarantee that you’re fertile, because there can be other reasons for infertility.
If you have a very low sperm concentration, you might still be able to get pregnant naturally.
Many factors can affect a couple’s chance of getting pregnant, including the couple’s frequency and timing of sex, the length of time the couple has tried to get pregnant, and the age and fertility of the female partner. Your semen analysis needs to be looked at together with other clinical information by your doctor.
Semen Ejaculate Volume
What It Is: Semen is made up of more than just sperm. In fact, less than 5% of semen is made up of sperm.
Healthy semen includes fluid from:
- The bulbourethral glands (which contains mucus to help the semen swim)
- The prostate gland (which includes zinc-rich fluid to maintain DNA stability of the sperm)
- The seminal vesicles (which includes important nutrients for the sperm)
- The testes (where the sperm come from)
What Is Considered Normal: Normal semen ejaculate is between 1.5 milliliters to 6 milliliters of fluid (about one-third of a teaspoon to a little over a teaspoon).
What Might Be Wrong If Results Are Abnormal: Low semen volume can be caused by an obstruction of the vas deferens (the duct that carries sperm from the testicles to the urethra), absence, or blockage of the seminal vesicle, partial retrograde ejaculation, or a hormonal imbalance.
Low volume can also be caused by stress over the test. If you are anxious about the test, talk to your doctor about ways to reduce your anxiety.
An abnormally high volume could be caused by inflammation of the reproductive glands.
Sperm Concentration
What It Is: Sperm concentration is the number of sperm found in one milliliter of semen.
What Is Considered Normal: There should be at least 15,000,000 (or 15 x 10^6) sperm per millimeter.
What Might Be Wrong If Results Are Abnormal: Low sperm concentration may be part of an overall low sperm count. It could also be related to an abnormally high ejaculate volume.
Motility
What It Is: Motility is the percentage of sperm who move. For fertilization to occur, sperm must swim up the female reproductive tract to meet the egg. Being able to swim to their destination is essential. Total motility refers to any movement, while progressive motility refers to the forward movement in either a line or in a large circle.
What Is Considered Normal: At least 40% of the sperm should be moving, and at least 32% should swim in a forward movement or in large circles.
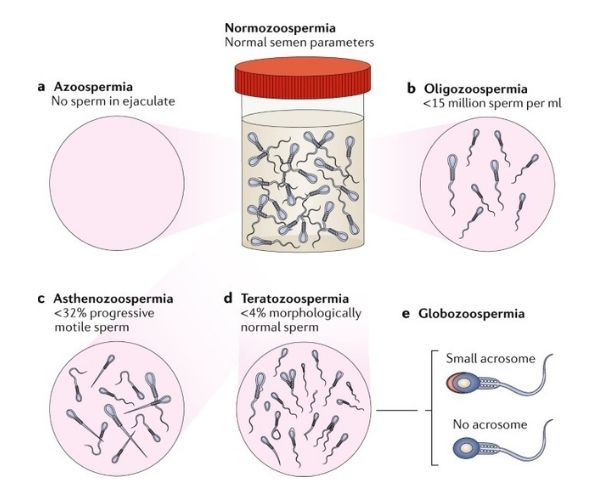
What Might Be Wrong If Results Are Abnormal: Asthenozoospermia is the term used for poor sperm motility. Poor sperm motility may be caused by illness, certain medications, nutritional deficiencies, or poor health habits like smoking. Many of the causes of low sperm count can also cause poor motility. Often the cause is never found.
Viability or Vitality
What It Is: Sperm viability refers to the percentage of live sperm in the semen sample. This is especially important to measure if sperm motility is low, to differentiate between live non-motile sperm and dead sperm.
What Is Considered Normal: At least 58% of the sperm cells should be viable.
What Might Be Wrong If Results Are Abnormal: Necrozoospermia is the term used when all sperm in the semen sample is dead. There are a variety of causes for necrozoospermia, including many of the same things that can cause low sperm count.
Using a non-fertility-safe lubricant or regular condom can kill sperm, even if they don’t contain spermicide. Make sure you tell your doctor if you used lubricant or a regular condom to produce your semen sample.
Ask your doctor about fertility-approved lubricants and specialty condoms that are available for the collection of semen samples.
Morphology
What It Is: Sperm morphology refers to the shape of the sperm cells. The lab technician closely examines a sample of sperm, checking to see approximately what percentage has a normal shape. The head, midsection, and tail are evaluated, as well as the measurements and proportions between each.
Before 2010, the World Health Organization had different requirements for sperm to be considered “normal” in shape. Labs may have evaluated sperm morphology according to the WHO criteria, or what is known as Kruger’s Strict criteria.
However, the WHO’s 2010 guidelines encourage the use of Kruger’s Strict criteria, based on the research of Thinus Kruger and Roelof Menkveld.4 Speak to your doctor to find out if they are using the outdated WHO criteria or Kruger’s criteria.
What Is Considered Normal: At least 4% should have a normal shape.
What Might Be Wrong If Results Are Abnormal: Teratozoospermia is the term used for poor sperm morphology. Poor sperm morphology may be caused by the same things that can cause low sperm counts.
Sperm morphology is poorly understood, and because the evaluation is somewhat subjective, scores can vary on the same semen sample, in the same lab, using the same scoring techniques.
If sperm morphology is abnormal, but all the other semen parameters fall within normal limits, then male fertility could still be considered normal.
Liquefaction
What It Is: When semen is ejaculated, it is thick and gelatinous. This is to help it adhere to the cervix. The semen eventually liquefies to enable the sperm to swim better.
What Is Considered Normal: Semen should liquefy within 20 to 30 minutes of ejaculation.
What Might Be Wrong If Results Are Abnormal: Delayed liquefaction may indicate a problem with the prostate, the seminal vesicles, or the bulbourethral glands, which are also known as the male accessory glands.
If delayed liquefaction occurs, your doctor might want to follow up with a post-coital test (PCT). This fertility test evaluates a female partner’s cervical mucus after sexual intercourse. If sperm are found and moving normally, the delayed liquefaction is not considered a problem.
Semen pH
What It Is: Semen pH is a measurement of how acidic or alkaline the semen is. The seminal vesicle fluid should be more alkaline, while the prostate fluids should be more acidic. In combination, they balance each other out in the semen.
Semen that is too acidic may kill the sperm or prevent fertilization.
What Is Considered Normal: The semen should have a pH greater than 7.2. Currently, there’s no consensus on how more alkaline semen may affect fertility, and so there’s no upper pH limit according to the WHO guidelines.
What Might Be Wrong If Results Are Abnormal: Usually, low pH is accompanied by other abnormal measurements, including a low volume of semen or low sperm counts. This may point to an obstruction or absence of the vas deferens.
White Blood Cells (WBC)
What It Is: White blood cells are the cells that fight infection in the body. All semen includes white blood cells.
What Is Considered Normal: The white blood cell count should be less than 1,000,000 per milliliter of semen, or 1.0 x 10^6 per ml.
What Might Be Wrong If Results Are Abnormal: A higher than normal white blood cell count (leukocytospermia) may indicate an infection. Bacterospermia is when excessive levels of bacteria are found in semen.
Anywhere from 5% to 20% of men tested may be found to have leukocytospermia.
Some men may have leukocytospermia and not have any active infection or male fertility impairment. There is a theory that a possible cause of bacterospermia is untreated dental infections, though this has not been proven.
If Your Results Are Abnormal
One abnormal semen analysis result is not necessarily a sign of impaired male fertility. Because so many factors can lead to a poor result, including recent illness or even stress over the test, your doctor will likely repeat the semen analysis in a few weeks.
Speak to your doctor about what to expect next. Be sure to disclose any possible causes for poor results (including recent illness, a love of hot tubs or heated car seats, trouble producing a sample for the analysis, and all the medications you’re currently taking, including any recreational drugs.)
If the poor results repeat, what treatments may be available? This depends on the cause of infertility as well as the female partner’s fertility and age.
There are some options for treatment.1 You might consider one or more of the following:
- Hormone treatments. It is not very common, but in some cases, hormonal treatment may help improve sperm count.
- IUI. Intrauterine insemination is a treatment where the man produces a semen sample, the sample goes through a special washing process, and then the specially washed semen is pushed through a catheter via the cervix into the woman’s uterus.
- IVF or IVF with ICSI. In IVF treatment, sperm and egg are put together in a lab, hopefully forming an embryo. Then, the embryo is transferred to the woman’s uterus. In conventional IVF, the sperm are put together with an egg in a petri dish. With IVF-ICSI, a single sperm cell is directly injected into an egg. There are additional risks and costs with ICSI, but it may be the only option for men with very low sperm count.
- Lifestyle change. If any poor health habits might be leading to lower sperm counts, those should be eliminated as soon as possible.
- Sperm donor. In some situations, it may be recommended to consider using a sperm donor.
- Surgery. If there is a varicocele (a varicose vein in the scrotum or testicle), removing it may improve sperm counts. Micro-surgical repair may be considered in some cases of male infertility, especially if it’s a vasectomy reversal.
- Testicular sperm extraction. In cases of extremely low sperm count, zero sperm count, or no ejaculate, a testicular sperm extraction is an option. This is when mature or immature sperm cells are extracted via a needle from the testicles. IVF with ICSI is required if this procedure is done.
- Treating any underlying medical conditions. Untreated celiac disease, diabetes, or a thyroid imbalance can all increase the risk of male infertility.
Get in Touch
Tell us about your problems and we’ll figure out the best treatment option for you.
Life Plus hospital
Women and Child Care Hospital in Indiranagar | LifePlus Hospital
At Life plus hospital, we offer a comprehensive range of women’s health services. The Department is managed by highly experienced lady gynecological doctors who offer specialized attention and compassionate care for women
Let's Schedule Your Appointment
IUI & IVF Success Story
https://youtu.be/3sBjEYtzV2Y
Semen Analysis Faq's
A semen analysis is used to determine whether a man might be infertile—unable to get a woman pregnant. The semen analysis consists of a series of tests that evaluate the quality and quantity of the sperm as well as the semen, the fluid that contains them. The test may be used, in conjunction with other infertility tests, to help determine the cause of a couple’s inability to get pregnant (conceive) and to help guide decisions about infertility treatment.
The semen analysis also can be used to determine whether sperm are present in semen after a man has had a vasectomy, a surgical procedure that prevents sperm from being released within the ejaculate. This surgery is considered a permanent method of birth control (99.9%) when performed successfully.
A semen analysis is performed when a healthcare practitioner thinks that a man or couple might have a fertility problem. Infertility is typically diagnosed when a couple has tried to get pregnant for 12 months without success.
A semen analysis to determine fertility should be performed on a minimum of two samples collected within 2 to 3 week intervals. Sperm count and semen consistency can vary from day to day, and some conditions can temporarily affect sperm motility and numbers.
When a semen analysis shows abnormal findings, the test is repeated at intervals as determined by the healthcare practitioner.
A shorter version of a semen analysis, a sperm check, is typically ordered about 3 months following a vasectomy to confirm success of the procedure and may be repeated as necessary until sperm are no longer present in the semen sample.
About one-third of cases are due to men’s problems with fertility, another third are due to women’s problems, and the remaining cases are due to a combination of men’s and women’s infertility issues or have no clear identifiable reasons for infertility.
Yes, there is a home test available that measures sperm count and gives a result within a few minutes. However, it is important to understand that a sperm count is only one part of a semen analysis for determination of male fertility and is only one aspect of a complex process. For more about home tests, including the benefits and cautions, see the article With Home Testing, Consumers Take Charge of Their Health.